What Is the Pathology of Corneal Disease?

The cornea is like a window that allows light to enter the eye. A dome-shaped surface, the clear cornea covers the front of the eye, which protects it from getting damaged. Our corneas also help us with focusing vision. However, when a cornea becomes diseased, it can lead to significant visual impairment and even blindness if not treated promptly.
With that in mind, let’s look—if you’ll pardon the pun—a little more closely at the conditions that make up the pathology of corneal disease.
Common Causes of Corneal Disease
Corneal disease can arise from a multitude of factors, with each affecting the cornea differently:
- Infections: Bacterial, viral, fungal, or parasitic infections can lead to conditions like keratitis (inflammation of the cornea). Herpes simplex virus, for instance, is a common culprit behind viral keratitis, which can cause recurrent ulcers and scarring.
- Injuries: Trauma to the eye, such as a scratch or a blow, can damage the cornea. Even minor injuries can lead to complications if not properly treated, potentially resulting in scarring or infection.
- Degenerative Conditions: Diseases like keratoconus, where the cornea thins and begins to bulge outward into a cone shape, can severely distort vision. Fuchs' dystrophy, another degenerative condition, affects the endothelium, leading to corneal swelling and clouding.
- Autoimmune Diseases: Conditions like rheumatoid arthritis or lupus can cause inflammation that may extend to the cornea, leading to complications like peripheral ulcerative keratitis.
- Nutritional Deficiencies: Vitamin A deficiency, for instance, can lead to xerophthalmia, a condition that causes dryness and thickening of the cornea, potentially leading to blindness.
- Genetic Factors: Some corneal diseases, such as certain types of dystrophies, are hereditary. These conditions often involve the gradual clouding of the cornea over time.
How Corneal Disease Develops
Corneal disease often begins with damage or disruption to one or more layers of the cornea. The specific pathology of the disease depends on the underlying cause and the area of the affected cornea.
Inflammatory Responses
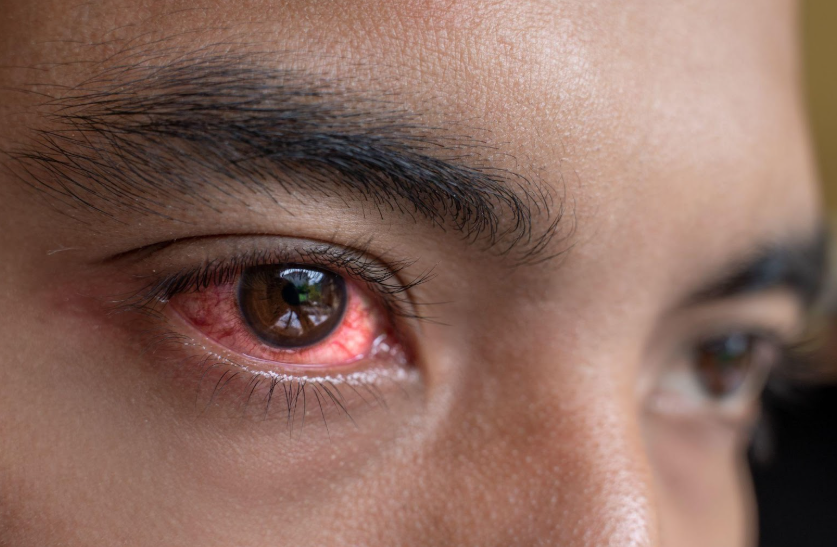
Many corneal diseases involve inflammation, which is the body's natural response to injury or infection. In the case of infectious keratitis, for example, bacteria, viruses, or fungi invade the cornea, triggering an inflammatory response. This response is characterized by redness, pain, and often, a discharge from the eye. If the infection penetrates deeply, it can lead to the formation of corneal ulcers, which are open sores on the cornea. These ulcers can cause scarring, leading to permanent vision impairment if not treated promptly.
Degenerative Changes
Degenerative corneal diseases, like keratoconus, involve progressive changes to the cornea’s structure. In keratoconus, the collagen fibers in the stroma weaken, causing the cornea to thin and bulge outward. This distortion interferes with the cornea's ability to focus light, leading to blurred and distorted vision. In advanced stages, scarring may occur, further compromising vision and sometimes necessitating a corneal transplant.
Corneal Dystrophies
Corneal dystrophies are a group of genetic, often hereditary, disorders that lead to the gradual clouding of the cornea. These conditions typically affect both eyes and progress slowly over time. For example, in Fuchs' dystrophy, the endothelium gradually deteriorates, leading to fluid buildup in the cornea. This causes swelling (edema) and eventually results in corneal haze, making vision cloudy. Other dystrophies, like lattice dystrophy, involve the deposition of abnormal proteins in the cornea, creating a lattice pattern of opacities and leading to recurrent erosions and scarring.
Autoimmune-Related Pathology
Autoimmune diseases can also affect the cornea, leading to conditions like peripheral ulcerative keratitis (PUK). In PUK, the body’s immune system mistakenly attacks the corneal tissue, causing ulceration and thinning at the edge of the cornea. This condition is often associated with systemic autoimmune diseases like rheumatoid arthritis. The inflammation and subsequent tissue damage can be severe, sometimes resulting in perforation of the cornea if left untreated.
The Impact on Vision
The impact of corneal disease on vision varies depending on the severity and location of the condition. Diseases affecting the central cornea tend to have the most significant impact on vision. For instance, a central corneal ulcer or scar can cause severe blurring, halos, or glare. In contrast, conditions that affect the peripheral cornea may have less impact on visual acuity but can still lead to discomfort and other complications.
Corneal diseases that cause scarring, clouding, or irregularities in the corneal surface can also lead to astigmatism, where the cornea’s shape becomes distorted, causing blurred or double vision. In some cases, the cornea becomes so damaged that it requires surgical intervention, such as a corneal transplant, to restore vision.
Diagnosis and Treatment
Diagnosing corneal disease typically involves a comprehensive eye examination, including a slit-lamp exam, which allows the eye care professional to closely examine the cornea and other parts of the eye. Additional tests, such as corneal topography (which maps the curvature of the cornea) or endothelial cell counts, may be necessary to diagnose specific conditions.
Treatment for corneal disease depends on the underlying cause like:
- Infections: Antibiotics, antiviral, or antifungal medications are used to treat infections, often in the form of eye drops. Severe infections may require oral medications or even surgery.
- Inflammatory Conditions: Steroid eye drops are commonly prescribed to reduce inflammation. In autoimmune-related corneal disease, systemic immunosuppressive therapy may be necessary.
- Surgical Interventions: In cases of severe damage, corneal transplants or procedures like corneal cross-linking (for keratoconus) may be required to restore or preserve vision.
- Management of Degenerative Diseases: For conditions like keratoconus, rigid gas-permeable contact lenses may help improve vision, while more advanced cases might need surgical interventions.
If you are suffering from blurred vision and redness around your eyes, don’t wait any longer! Our team at South Shore Eye Care can help you get your corneas back in working order in no time. Contact us today to request an appointment!