Recognizing and Treating Herpes Simplex Keratitis in the Eyes
Herpes Simplex Keratitis (HSK) is the leading cause of infectious corneal blindness in developed countries. Caused primarily by Herpes Simplex Virus Type 1 (HSV-1), this condition can cause recurrent corneal inflammation, ulceration, and even permanent vision loss if untreated.
What Is Herpes Simplex Keratitis?
HSK is a corneal infection that results from the reactivation of HSV-1. The virus typically enters the body during childhood and remains dormant in the trigeminal ganglion. While the initial infection may go unnoticed, the virus can later reactivate due to triggers like stress, fever, ultraviolet light exposure, ocular trauma, or immunosuppression.
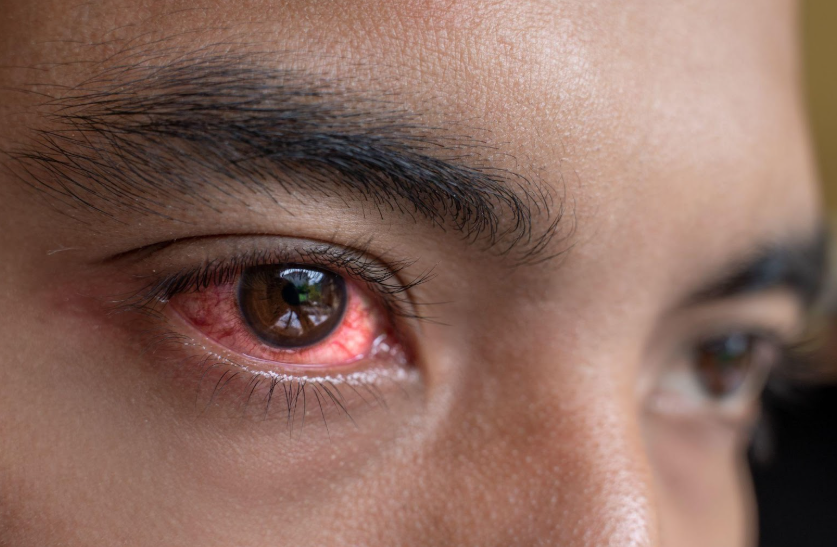
Recognizing the Clinical Signs of HSK
While some symptoms of herpes simplex keratitis (HSK) can be mistaken for other eye conditions, HSV is the cause of HSK. These include red eyes, tearing, irritation, and mild pain. You may also have blurry vision, light sensitivity, or feel like something is in your eye.
Your doctor might discover a branching sore on your cornea while performing an examination. Moreover, your eye might feel less sensitive than usual. If you have experienced HSV or cold sores in the past, notify your eye doctor immediately.
The Overlooked Role of Allergies in Corneal Vulnerability
Though HSV causes HSK, allergies can increase your susceptibility by compromising the protective barrier of the ocular surface. Common allergic conditions like allergic conjunctivitis and eyelid eczema often lead to inflammation, itching, and frequent eye rubbing—making it easier for HSV to reactivate or worsen.
Allergies That Complicate Your Eye Health
Inflammation, itching, and frequent rubbing can damage the surface of your eyes and create a path for HSV to reactivate. Managing your allergies helps protect your eyes from further irritation and infection. To lower your risk, treat your allergies with prescribed antihistamines, mast cell stabilizers, or anti-inflammatory drops.
Allergic conjunctivitis causes rubbing that harms your cornea
When your eyes itch from allergic conjunctivitis, it’s natural to rub them. But rubbing causes tiny injuries to your cornea, which can lead to swelling, irritation, and a higher risk of viral reactivation. If you have a history of HSV, this increases the chance of another outbreak.
Eyelid eczema exposes your eyes to more triggers.
If you have eczema on your eyelids, the skin becomes dry and irritated. Touching or scratching the area often spreads bacteria, allergens, and viruses to your eyes. This makes it easier for HSV to reactivate and cause keratitis.
Contact dermatitis from products weakens your eye’s defense
Some eye drops, makeup, or skin products can trigger allergic reactions around your eyes. These reactions damage the surface and make it harder for your eyes to protect themselves. This gives HSV a chance to reactivate more easily.
Eye Rubbing as a Hidden Risk for Viral Reactivation
The mechanical stress from rubbing not only disrupts the corneal epithelium but may also trigger HSV reactivation in the trigeminal ganglion. It also increases your risk of other eye conditions, particularly when combined with dry eye, allergies, or frequent screen use.
- Corneal Abrasions: Tiny surface tears that allow viral particles to penetrate deeper layers. These abrasions often go unnoticed but can create a pathway for infections like HSV to spread. If not treated quickly, they may lead to ulcers and delayed healing.
- Keratoconus: Progressive corneal thinning and distortion from chronic mechanical trauma. As the cornea weakens, your vision becomes more distorted and harder to correct with glasses. Early detection is key, as advanced cases may require specialty lenses or surgery.
- Styes and Preseptal Cellulitis: Introduction of bacteria from the hands to the eyelid margin. These infections cause swelling, pain, and redness around your eyelids and may spread if untreated. Frequent rubbing increases your risk, especially with poor hand hygiene.
- HSV Recurrence: Ocular stress is a known activator of latent HSV, especially when combined with inflammation or immune suppression.
When You Need Immediate Eye Care
If you develop sudden blurry vision, eye pain, or light sensitivity—especially with a history of cold sores or previous eye infections—you should see an eye doctor right away. Redness that keeps coming back or symptoms that worsen with steroid drops are also signs that need urgent attention. Delaying care increases the risk of scarring or permanent vision changes.
Shingles and the Risk of Vision Loss
Shingles (herpes zoster), another virus in the herpes family, can also affect the eye and lead to permanent vision loss if not treated promptly. If shingles appears on the head—especially near the eye—it’s critical to seek care immediately. At South Shore Eye Care, LLP, we strongly recommend coming in for an appointment if you develop shingles on the face or scalp.
Early evaluation and antiviral treatment can prevent serious eye complications.
How Doctors Diagnose Herpes Simplex Keratitis
Diagnosis begins with a thorough eye exam using a slit lamp to detect corneal ulcers and swelling. Fluorescein dye can reveal the branching ulcer pattern typical of HSV. Testing corneal sensitivity helps identify nerve damage caused by the virus.
In some cases, your doctor may use PCR testing to detect HSV DNA or confocal microscopy to view affected cells more closely. These tools help confirm the diagnosis and avoid misusing treatments like steroids.
Choosing the Right Treatment Based on Severity
Treatment of HSK is tailored to the depth and activity of the infection. Mismanagement can cause rapid worsening, especially when corticosteroids are used to treat active epithelial infections. Epithelial keratitis is treated with topical antiviral drops or gels and sometimes oral antivirals if needed. In certain cases, gently removing the infected tissue may help healing.
Stromal keratitis requires both corticosteroids and oral antivirals to manage inflammation without letting the virus reactivate. Endothelial keratitis is usually treated with steroid eye drops and longer courses of oral antivirals to prevent recurrence. All treatment should be guided by an eye specialist.
Preventing Recurrences and Long-Term Complications
Herpes simplex keratitis has a high chance of coming back, especially within the first five years after an initial episode. Taking daily oral antivirals like acyclovir can reduce the chance of recurrence. Managing allergies and avoiding eye rubbing helps keep the eye surface stable. UV-blocking sunglasses protect against light-triggered flare-ups.
Steroid eye drops should only be used under medical guidance as they can worsen infections. During active symptoms, avoid wearing contact lenses to prevent further irritation. For those with frequent episodes, long-term antiviral use may be needed even when symptoms aren’t present.
Whether you’re dealing with eye allergies, eyelid eczema, styes, or a confirmed HSV outbreak, personalized care can make all the difference. Our eye specialists at
South Shore Eye Care, LLP can guide you and offer advanced treatment options tailored to your visual health.
Schedule your comprehensive eye exam today!